‘Hidden’ NHS appointments waiting list exceeds 11MILLION – and it has soared 50% since Covid
More than 11 million people needing follow-up care in hospital are now languishing on ‘hidden’ NHS waiting lists, a study suggests.
Experts warn that these patients – equivalent to one in five of the population – are at risk of neglect and harm as health leaders prioritize higher profile cases.
The NHS publishes headline figures every month showing how many people are waiting to start treatment, with a record 7.75 million.
Rishi Sunak has made tackling this backlog one of his five priorities as prime minister, but the count excludes those who have undergone a procedure such as hip surgery or cataract removal and need vital checks.
New analysis by the reform think tank, based on freedom of information revelations, indicates there are 11.36 million patients waiting for follow-up appointments.
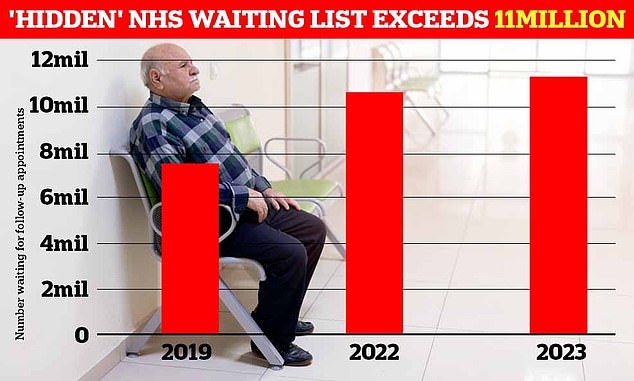
The think tank found that the waiting list for follow-up treatments has grown significantly since the pandemic. It is estimated that more than 11 million patients are waiting for continuing care – approximately 3.5 million more people than the elective backlog
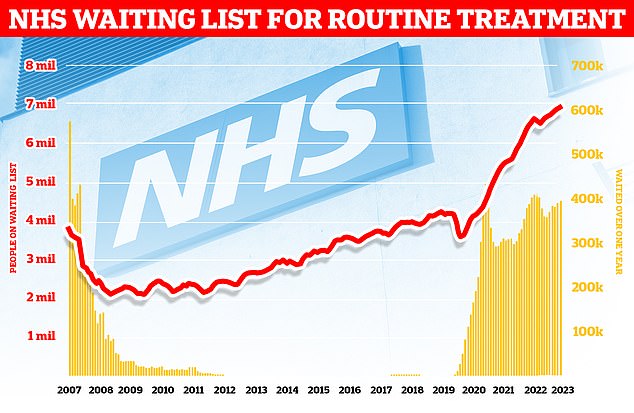
The widening backlog in England stood at 7.75 million in August – the equivalent of one in seven people. This includes nearly 400,000 people stuck in the system for more than a year, often in pain
It means that the ‘hidden’ waiting list has 3.6 million more patients than the elective waiting list, with a total of 19.1 million.
Each requires the attention of overburdened NHS staff, which could be used to treat new patients or monitor existing patients.
Failure to adequately monitor long-term conditions or cancer patients, failure to manage medications, and failure to monitor patients after surgery poses significant clinical risks.
The number of people waiting for follow-up care increased by 50 percent between May 2019, before the pandemic, and May this year.
Each trust has an average of 100,000 people on its ‘hidden’ list, but one trust has more than half a million.
Nearly half of trusts – 47 per cent – failed to provide data on their follow-up waiting lists.
Some 62 trusts provided data, 17 did not respond to the FOI request despite a legal duty to do so, and 39 claimed not to possess the information.
Sebastian Rees, senior research and co-author of the report at Reform, said: ‘Patients’ health and safety are threatened by these hidden waiting lists.
‘If follow-up appointments are not arranged on time, there is a risk that cancer recurrence or complications after surgery will go undetected, and people will become disabled due to a worsening condition.
‘It is deeply concerning that so many trusts cannot even tell us how many people are on their follow-up waiting lists, which shows a lack of priorities or understanding of the problem.
‘NHS England must require all trusts to report this data and hold hospitals accountable for tackling this hidden backlog.’
The minimum and maximum waiting lists in 2023 vary drastically.
Although East Kent Hospitals have doubled the number of outpatient referrals of Nottingham University Hospitals, suggesting greater acute confidence, their follow-up lag is 513 times that of Nottingham: 516,919 versus 1,008.
This suggests that some patients are receiving an unacceptably poor quality of care based on their counselor’s decision not to prioritize follow-up appointments, or due to inadequate management of follow-up waiting lists.
Ophthalmology has the highest number of waiters, with a 28.5 percent increase from 2019 to 2023, the data shows.
The Royal College of Ophthalmologists has previously warned that permanent damage from avoidable vision loss is nine times more likely in follow-up patients than in new patients.
Rachel Power, chief executive of the Patient Association, described the research as ‘alarming’.
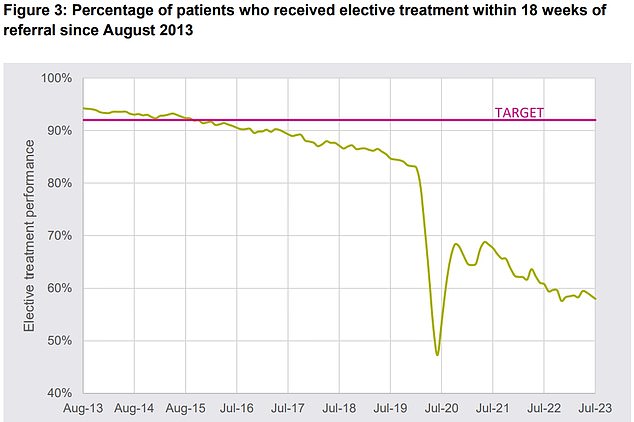
Under the NHS Constitution, at least 92 percent of patients must receive elective treatment within 18 weeks of initial referral (pink line). September 2015 was the last time this standard was met. NHS data for July shows that fewer than six in ten patients were seen within this time frame
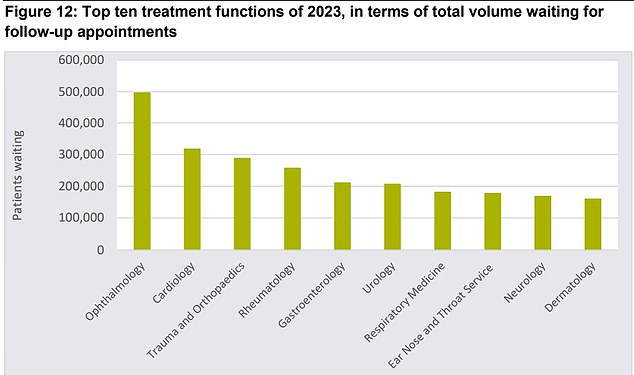
The graph shows the top ten treatment areas with the largest follow-up backlog in 2023. Most patients are waiting for a check-up appointment in ophthalmology, cardiology or orthopedics
She added: ‘We are concerned that long waits could lead to patients’ health deteriorating, perhaps to the point where treatment is no longer effective.
‘We urge the NHS to be transparent about the number of patients waiting for care.’
Saffron Cordery, deputy chief executive of NHS Providers, which represents NHS trusts, said: ‘No trust leader wants patients – their first priority – to have to wait for the care they need.
‘It is important to note that while the waiting list for follow-up appointments is concerning, many people on that list do not require urgent treatment or care.
‘Trusts work extremely hard to see patients as quickly as possible.’
Rory Deighton, director of the Acute Network at the NHS Confederation, which represents healthcare organisations, said: ‘Health leaders and their teams are doing everything they can to get the NHS back on its feet and reduce waiting lists despite serious challenges, but with industrial action that continue to hinder recovery efforts need more help to do so.”
An NHS spokesperson said: ‘These types of appointments are not part of the elective care waiting list, they are routine follow-up appointments after treatment has taken place, and in many cases patients can be booked for multiple appointments; it is therefore simply wrong to count these appointments as patients or to state that all follow-up patients wait longer than necessary.
‘Thanks to the hard work of staff, 87,000 more patients were treated in August than in the same month before the pandemic, while the NHS is also working to reduce the number of unnecessary appointments, with thousands of patients deciding they don’t need to actually attend .’
