REVEALED: How health insurers like CVS Health and Cigna charge more than 20 TIMES the market value for cancer drugs
Health insurers that own pharmacies charge themselves more than twenty times the market value for certain medications, causing patients to face significant out-of-pocket costs and premiums.
Insurance companies CVS Health and Cigna can pay pharmacies — which they often own — more than $6,600 a month for a cancer drug available for as little as $55 a month, according to a new report in The Wall Street Journal. All insurers mentioned said the analysis gave a limited view of the overall market.
“It’s a win-win situation,” Dr. Simon F. Haeder, associate professor in the Department of Health Policy and Management at Texas A&M University School of Public Health, told DailyMail.com.
“The insurance company has an interest in getting as much out of the patient as possible, which is money that they can get from their own payments in addition to the premiums they collect,” Haeder said.
CVS Health charges $7,000 a month for the cancer drug Gleevec. The same dose can be purchased elsewhere for about $50
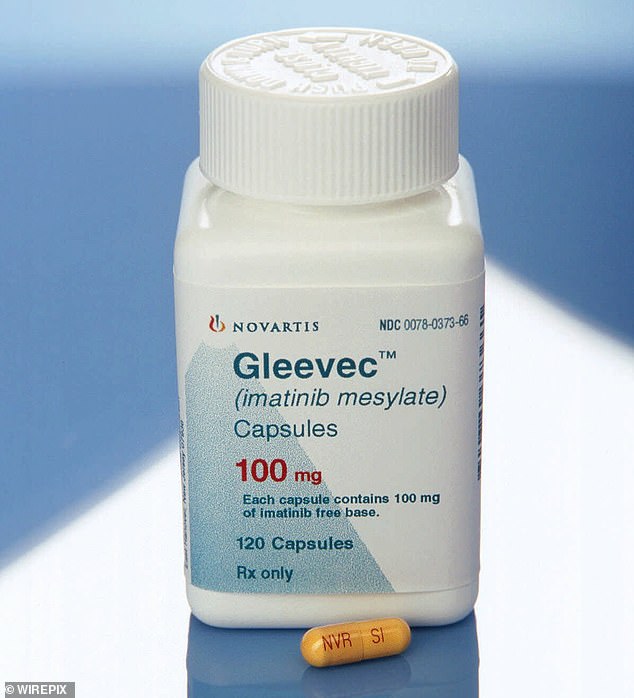
CVS, Cigna and UnitedHealth can charge significantly more than market value for drugs, meaning patients pay significant out-of-pocket costs and premiums rise. Gleevec (pictured) is an anti-cancer drug and has a market value of about $50 per month
The drugs most affected by this phenomenon are known as generics. When the patent for a particular drug expires, it can be copied by other manufacturers – usually at very low cost. Generic drugs are intended to be a useful way to reduce the high costs of medicines.
But for a selection of generic drugs, the Journal found that CVS and Cigna prices were, on average, at least 24 times higher than what the manufacturers of those drugs sell them for.
Cancer drug Gleevec has a market value of about $50 per month. CVS Health will buy it for $7,000 and Cigna will pay about $6,600. A third insurer, UnitedHealth, charges about $200 per month, according to the Journal.
Generics of the lung cancer drug Tarceva can be purchased for about $70 per month. CVS, Cigna and UnitedHealth pay approximately $2,050, $4,400 and $550, respectively.
“Generic drugs tend to be relatively cheap in Europe, but in the US, something being generic doesn’t necessarily mean it’s much cheaper than the original version,” says Haeder.
He says that the scheme is aimed at extracting as much money as possible from the patient in various ways.
The most obvious is that by purchasing the drugs at higher prices, the insurer can charge the patient more when he goes to pick up the drugs.
That may be because the terms of their plan require them to pay a co-pay – a fixed portion of the cost of their medication – or because they pay for medications up to a certain deductible above which the insurer will pay.
Second, this setup not only makes insurers more money now, but also allows them to increase profits later. When premiums need to be renegotiated, they can point to the patient’s previous spending on medications and justify more expensive follow-up coverage, Haedar said.
The Affordable Care Act requires insurance companies to spend at least 85 percent of the revenue they receive from medical care premiums. If they don’t, they have to pay customers rebates on those premiums.

Generics of the lung cancer drug Tarceva (pictured) can be purchased for about $70 per month. CVS, Cigna and UnitedHealth pay approximately $2,050, $4,400 and $550 respectively
The prescription drug supply chain is notoriously complex and consists of a variety of parties that are often not only aligned, but often own each other.
In addition to the insurer and the pharmacy, there is a so-called PBM, or pharmacy benefit manager. They negotiate with the pharmacy about reimbursement for the medications and discounts from the drug manufacturer.
Drug manufacturers are incentivized to pay for these rebates because the PBM will in turn recommend the drug to consumers.
The nation’s three largest PBMs – Caremark, Evernorth/Express Scripts and OptumRx – are owned by CVS Health, Cigna and UnitedHealth, respectively. Control 85 percent of the market.
So everyone in the supply chain – except the consumer – makes money as a result of a higher list price of the drug.
“The incentive is there for the PBMs and the specialty pharmacies to keep prices as high as possible,” Shannon Ambrose, the co-founder of Archimedes, a company that competes with PBMs, told the Journal.
A spokesperson for CVS Health told DailyMail.com: ‘Comparing prices for a limited number of generic drugs provides an incomplete picture because Medicare plans price their network offerings for all prescription drugs – brand, generic and biosimilars – to the costs for the most expensive branded products.
“This market basket approach reduces brand costs, lowering overall costs for plan sponsors and members.”
He added that the prices the company submits to Medicare represent the highest contracted rate it has with pharmacies and do not include the lower prices that some of its pharmacies may accept.
Responding to The Journal’s report, Cigna told DailyMail.com: ‘This misleading analysis does not accurately reflect typical drug costs for our customers. This article singles out isolated medications from the thousands we cover and does not provide meaningful insights into the affordability and safety of medications we guarantee for millions of people.”
DailyMail.com also wrote to UnitedHealth for comment on the prices it pays per month for cancer drugs, but did not receive a response at the time of publication. It told the Journal that none of the medications listed are commonly used by the patient population and that most would pay less out of pocket through the insurance plan.
